SURGICAL AWARENESS FOR COMMUNITY
“Time and health are two precious assets that we don’t recognize and appreciate until they have been depleted.”
Awareness of disease and symptoms is essential for screening and early detection. If members of the public are aware of a disease and its symptoms, they are more likely to take action to prevent it from happening to them or go to healthcare providers for check-ups.
Creating a health awareness campaign is an effective way to prevent the spread of diseases affecting your community. The community you live in is part of who you are. Even if you don’t see your neighbors every day, you recognize that the decisions you make impact those around you. You’re all in it together, and you wouldn’t have it any other way! Improving your community and helping others is often at the top of your mind. So when the phrase “community health” crossed your radar, you had to know more. What is community health? And how does it affect the lives of those in your area? Community health is the intersection of healthcare, economics, and social interaction. Unfortunately, many people are unaware of the role this type of healthcare plays in their everyday lives.

Adequate awareness of vascular diseases and their risk factors may help reduce the population’s exposure to modifiable risk factors and thereby contribute to prevention and control strategies. There is limited data on knowledge among the general population in third-world countries regarding diseases and risk factors.
September is National Vascular Disease Awareness Month. Vascular diseases, which include arterial disease, venous disease, and blood clots, are major health concerns. The spotlight on vascular disease calls attention to one of the leading causes of death around the globe.

Understanding Vascular Disease
Vascular disease refers to any condition that affects your circulatory system 一 the vast network of arteries and veins in your body. Individuals of all ages, genders, and races are at risk for developing vascular diseases, but certain risk factors can increase your risk of having a problem with your blood vessels. Age, family history of vascular disease, obesity, sedentary lifestyle, and certain underlying health conditions (such as type 2 diabetes) all increase your risk for developing one of these conditions.
Examples of vascular diseases include:
- Arterial diseases, such as peripheral artery disease (PAD), renal artery disease, popliteal entrapment syndrome, and carotid artery disease
- Venous disease, including varicose veins, spider veins, and chronic venous insufficiency
- Blot clots, including pulmonary embolism and deep vein thrombosis (DVT)
- Aortic aneurysm
- Blood clotting
- disorders
- Lymphedema
Vascular diseases can lead to complications if they aren’t treated. Some may require immediate treatment (such as an aortic aneurysm) while others can slowly worsen over time. Regardless, any disease that impacts the health and function of your veins or arteries should be taken seriously.
“A fit body, a calm mind, a house full of love. These things cannot be bought – they must be earned.”
Vascular surgery?
Vascular surgery is a surgical subspecialty in which diseases of the vascular system, or arteries, veins, and lymphatic circulation, are managed by medical therapy, minimally-invasive catheter procedures, and surgical reconstruction. The specialty evolved from general and cardiac surgery and includes treatment of the body’s other major and essential veins and arteries. Open surgery techniques, as well as endovascular techniques, are used to treat vascular diseases. The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system excluding the coronaries and intracranial vasculature.
Vascular surgery encompasses the diagnosis and comprehensive, longitudinal management of disorders of the arterial, venous, and lymphatic systems, exclusive of the intracranial and coronary arteries. Diplomates in vascular surgery should have significant experience with all aspects of treating patients with all types of vascular disease, including diagnosis, medical treatment, and reconstructive vascular surgical and endovascular techniques. Diplomates in vascular surgery should possess the advanced knowledge and skills to provide comprehensive care to patients with vascular disease, understand the needs of these patients, teach this information to others, provide leadership within their organizations, conduct or participate in research in vascular disorders, and demonstrate self-assessment of their outcomes.
What do vascular surgeons do?
Vascular surgeons are specialists who are highly trained to treat diseases of the vascular system. Your blood vessels –arteries carrying oxygen-rich blood and veins carrying blood back to the heart — are the roadways of your circulatory system. Without smoothly flowing blood, your body cannot function. Conditions such as the hardening of the arteries can create “traffic jams” in your circulatory system, obstructing the flow of blood to any part of the body.

The vascular surgeon must have advanced knowledge and experience with the management of vascular problems including:
- All elements of clinical evaluation; non-invasive testing including plethysmography, duplex ultrasonography, magnetic resonance imaging, CT scans, angiography, and other diagnostic tests utilized in the diagnosis of vascular disease.
- Comprehensive management of vascular disease to include screening and surveillance, medical management, drug therapy, risk factor management, wound management including amputations, and other adjunctive procedures.
- Indications and techniques relating to open and endovascular treatment of vascular disorders to include the entire spectrum of interventions used to treat vascular disorders including occlusive, aneurysmal, inflammatory disease, trauma, and neurovascular compressive syndromes involving the arteries and veins of the body (excluding the intracranial and coronary arteries). This includes the aorta and its branches, the arteries of the neck, pelvis and upper and lower extremities, and the venous system.
- The critical care of the vascular surgery patient.
Types of Vascular Surgery
There are various types of vascular surgery, depending on the problem you have. Listed below are some of the conventional techniques for addressing issues affecting your vascular system.
1. Angioplasty and Stenting
Angioplasty and stenting is a minimally invasive procedure in which your surgeon opens a narrowed artery using a catheter-guided balloon. This procedure treats conditions that include:
- Carotid artery disease, a narrowing of the blood vessels that carry oxygenated blood from the heart to the brain
- Peripheral artery disease, a narrowing of the blood vessels that carry oxygenated blood to the arms and legs
2. Atherectomy
Atherectomy in another minimally invasive procedure in which a specialized catheter is inserted into a blocked artery that allows your vascular surgeon to cut and remove plaque from within your blood vessels. This method can be used to treat patients with peripheral artery disease and allows vascular access for patients who need dialysis.
3. Arteriovenous (AV) Fistula
During an AV fistula procedure, your vascular surgeon connects a vein in your forearm directly to an artery. This makes the vein stronger and wider, and more easily to be accessed for patients with kidney failure who require dialysis.
4. Arteriovenous (AV) Graft
Similar to AV fistula procedure that creates an access point for dialysis, an AV graft procedure also involves surgically connecting an artery to a vein – but in this case, via a synthetic tube (the “graft”).
5. Open Abdominal Surgery
Open abdominal surgery involves making a small incision to repair an aortic aneurysm or blockage of the aorta (the artery that travels from your heart down to the pelvis) where it passes through the abdomen. In many cases, your vascular surgeon will suture a graft into the aorta to redirect blood flow around the problem area.
6. Thrombectomy
A thrombectomy is a procedure to remove a blood clot from a vein or artery. It is done to restore proper blood flow and prevent life-threatening complications such as when a blood clot travels to the lungs (pulmonary embolism) or brain, which can cause a stroke. Angioplasty and stenting may also be performed at the same time as a thrombectomy.
7. Vascular Bypass Surgery
Bypass grafting is a surgical treatment that focuses on creating an alternate channel for blood flow, bypassing a damaged vessel.
This surgery may be used to treat patients with the following disorders:
- Vertebrobasilar disease, affecting blood flow to the back of the brain
- Peripheral artery disease, affecting blood flow to the arms and legs
- Renal vascular disease, affecting blood flow to the kidneys
- Mesenteric vascular disease, affecting blood flow to the intestines
8. Open Carotid and Femoral Endarterectomy
Open carotid and femoral endarterectomy involve the surgical removal of plaque within the inner lining of the arteries feeding blood to your brain or legs, respectively. This surgery is performed in cases of moderate to severe blockage.
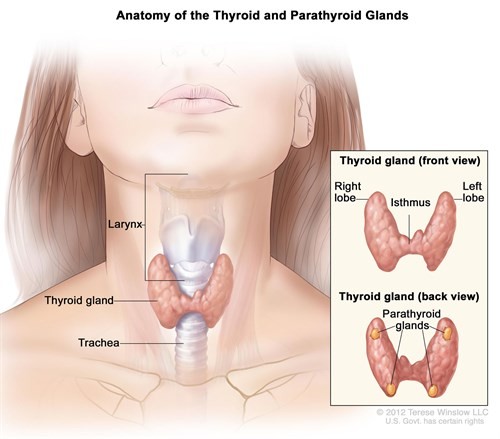
Thyroid Surgery
The thyroid gland is a butterfly-shaped organ composed of two cone-like lobes or wings connected via the isthmus. The gland regulates metabolism by secreting hormones. When diseases affect the thyroid, its size or activity may become abnormal.
What is a Thyroidectomy?
A thyroidectomy is a surgical procedure to remove all or part of the thyroid gland and is used to treat diseases of the thyroid gland including:
- Thyroid cancer
- Hyperthyroidism (overactive thyroid gland)
- Large goiters or thyroid nodules cause symptomatic obstruction such as swallowing or breathing difficulties.
- Multi-nodular Goiter
A thyroidectomy is traditionally a minimally invasive surgery performed through a small horizontal incision in the front of the neck. The entire thyroid gland may be removed or just a single lobe, a portion of a lobe, and the isthmus or other structures. Depending on the extent of the operation, patients may need to take the drug levothyroxine, an oral synthetic thyroid hormone.
Thyroid Thermal Ablation
Thermal ablation is a minimally invasive technique that is gradually acknowledged as an effective alternative to surgery to treat thyroid nodules. Benign thyroid nodules (BTNs) affect 18.6% of citizens worldwide , and have a negative effect on quality of life . In China, BTNs are seen in almost 33% of females and impose a heavy economic burden on society . Since medication therapy is rarely effective, the common intervention methods for BTNs include conventional thyroidectomy, endoscopic thyeoidectomy and thyroid thermal ablation .
The two most frequently-used treatment methods for BTNs are thermal ablation (microwave ablation, radiofrequency ablation and laser ablation) and conventional thyroidectomy. Thyroid ablation destroys the nodules thermally but conventional thyroidectomy removed the thyroid lobes. Thyroid thermal ablation does not leave a surgical incisions on the neck, takes less operative time, and allows patients early returns to routine life . Common methods applied for thyroid thermal ablation are radiofrequency ablation (RFA) and microwave ablation (MWA).
Similar to thyroid thermal ablation, total endoscopic thyroidectomy could also avoid obvious incisions on neck. But endoscopic thyroidectomy takes longer operative time and requires advanced endoscopic skills. And for patients undergoing endoscopic thyroidectomy, when post-operative haemorrhage occurs and an emergency surgery is needed, an incision on the neck would also be inevitable . Endoscopic thyroid lobe resection only requires a removal of the thyroid lobes containing TNs. The relative low popularity of endoscopic equipment also restricted endoscopic thyroidectomy.
Thyroid thermal ablation is superior to conventional thyroidectomy in terms of patients satisfaction, post-operative quality of life, and shorter hospital stay but takes longer to achieve BTNs volume reduction. The complication rates between the two groups were similar.
What is Cholesterol?
Cholesterol is a waxy, fat-like substance that’s found in all the cells in your body. Your body needs some cholesterol to make hormones, vitamin D, and substances that help you digest foods. Your body makes all the cholesterol it needs. Cholesterol is also found in foods from animal sources, such as egg yolks, meat, and cheese.
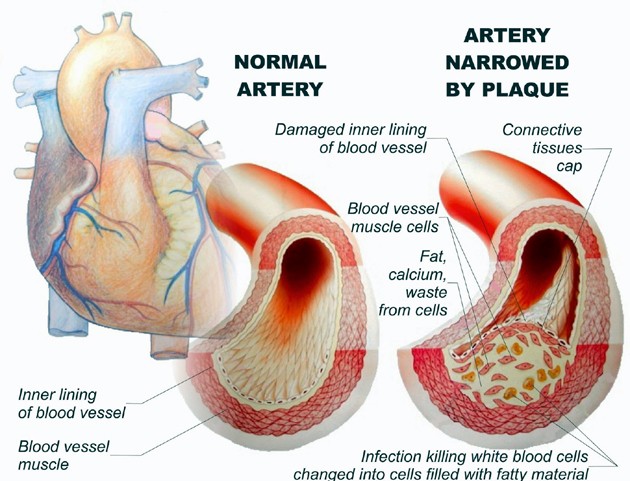
If you have too much cholesterol in your blood, it can combine with other substances in the blood to form plaque. Plaque sticks to the walls of your arteries. This buildup of plaque is known as atherosclerosis. It can lead to coronary artery disease, where your coronary arteries become narrow or even blocked
What are HDL, LDL, and VLDL?
HDL, LDL, and VLDL are lipoproteins. They are a combination of fat (lipid) and protein. The lipids need to be attached to the proteins so they can move through the blood. Different types of lipoproteins have different purposes:
- HDL stands for high-density lipoprotein. It is sometimes called “good” cholesterol because it carries cholesterol from other parts of your body back to your liver. Your liver then removes the cholesterol from your body.
- LDL stands for low-density lipoprotein. It is sometimes called “bad” cholesterol because a high LDL level leads to the buildup of plaque in your arteries.
- VLDL stands for very low-density lipoprotein. Some people also call VLDL a “bad” cholesterol because it too contributes to the buildup of plaque in your arteries. But VLDL and LDL are different; VLDL mainly carries triglycerides and LDL mainly carries cholesterol.
What causes high cholesterol?
The most common cause of high cholesterol is an unhealthy lifestyle. This can include:
- Unhealthy eating habits, such as eating lots of bad fats. One type, saturated fat, is found in some meats, dairy products, chocolate, baked goods, and deep-fried and processed foods. Another type, trans fat, is in some fried and processed foods. Eating these fats can raise your LDL (bad) cholesterol.
- Lack of physical activity, with lots of sitting and little exercise. This lowers your HDL (good) cholesterol.
- Smoking, which lowers HDL cholesterol, especially in women. It also raises your LDL cholesterol.
Genetics may also cause people to have high cholesterol. For example, familial hypercholesterolemia (FH) is an inherited form of high cholesterol. Other medical conditions and certain medicines may also cause high cholesterol.
What health problems can high cholesterol cause?
If you have large deposits of plaque in your arteries, an area of plaque can rupture (break open). This can cause a blood clot to form on the surface of the plaque. If the clot becomes large enough, it can mostly or completely block blood flow in a coronary artery. If the flow of oxygen-rich blood to your heart muscle is reduced or blocked, it can cause angina (chest pain) or a heart attack. Plaque also can build up in other arteries in your body, including the arteries that bring oxygen-rich blood to your brain and limbs. This can lead to problems such as carotid artery disease, stroke, and peripheral arterial disease.
How is high cholesterol diagnosed?
There are usually no signs or symptoms that you have high cholesterol. There is a blood test to measure your cholesterol level. When and how often you should get this test depends on your age, risk factors, and family history. The general recommendations are:
For people who are age 19 or younger::
- The first test should be between ages 9 to 11
- Children should have the test again every 5 years
- Some children may have this test starting at age 2 if there is a family history of high blood cholesterol, heart attack, or stroke
For people who are age 20 or older::
- Younger adults should have the test every 5 years
- Men ages 45 to 65 and women ages 55 to 65 should have it every 1 to 2 years
How can I lower my cholesterol?
You can lower your cholesterol through heart-healthy lifestyle changes. They include a heart-healthy eating plan, weight management, and regular physical activity. If the lifestyle changes alone do not lower your cholesterol enough, you may also need to take medicines. There are several types of cholesterol-lowering drugs available, including statins. If you take medicines to lower your cholesterol, you still should continue with the lifestyle changes. Some people with familial hypercholesterolemia (FH) may receive a treatment called lipoprotein apheresis. This treatment uses a filtering machine to remove LDL cholesterol from the blood. Then the machine returns the rest of the blood back to the person.
Good and Bad cholesterol
 There are two types: high-density lipoprotein (HDL) and low-density lipoprotein (LDL). As a general rule, HDL is considered “good” cholesterol, while LDL is considered “bad.” This is because HDL carries cholesterol to your liver, where it can be removed from your bloodstream before it builds up in your arteries. LDL, on the other hand, takes cholesterol directly to your arteries. This can result in atherosclerosis, a plaque buildup that can even cause heart attack and stroke. When your body has too much LDL cholesterol, the LDL cholesterol can build up on the walls of your blood vessels. This buildup is called “plaque.” As your blood vessels build up plaque over time, the insides of the vessels narrow. This narrowing blocks blood flow to and from your heart and other organs. When blood flow to the heart is blocked, it can cause angina.
There are two types: high-density lipoprotein (HDL) and low-density lipoprotein (LDL). As a general rule, HDL is considered “good” cholesterol, while LDL is considered “bad.” This is because HDL carries cholesterol to your liver, where it can be removed from your bloodstream before it builds up in your arteries. LDL, on the other hand, takes cholesterol directly to your arteries. This can result in atherosclerosis, a plaque buildup that can even cause heart attack and stroke. When your body has too much LDL cholesterol, the LDL cholesterol can build up on the walls of your blood vessels. This buildup is called “plaque.” As your blood vessels build up plaque over time, the insides of the vessels narrow. This narrowing blocks blood flow to and from your heart and other organs. When blood flow to the heart is blocked, it can cause angina.
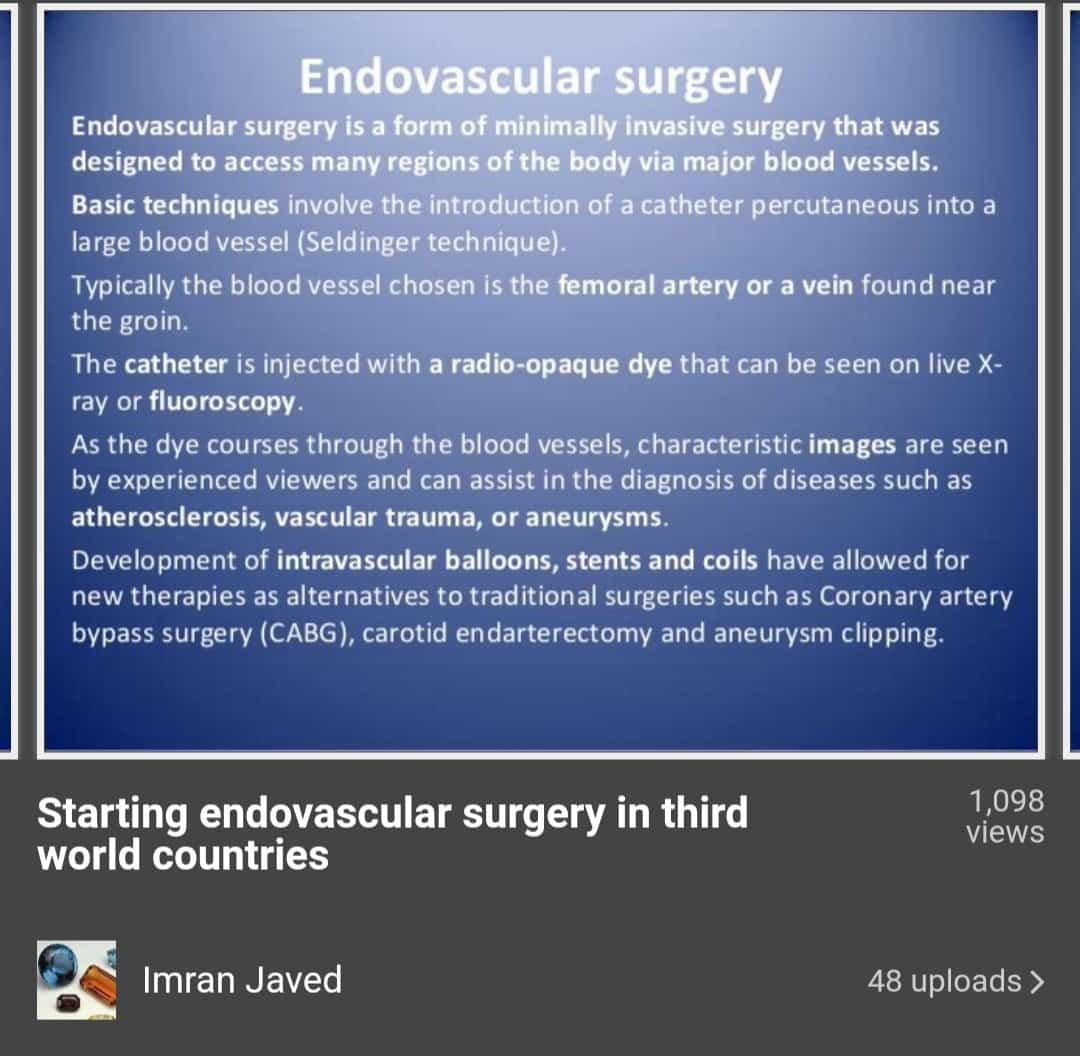
Endovascular Surgery in Third World Countries.
Endovascular therapy is a well-established treatment modality for a variety of cerebrovascular central nervous system disorders. The past few decades have witnessed dramatic improvements in the field of neuroendovascular surgery. These techniques are now used in the treatment of intracranial aneurysms, vascular malformations, carotid stenoses, intracranial vascular stenoses, and acute ischemic stroke.
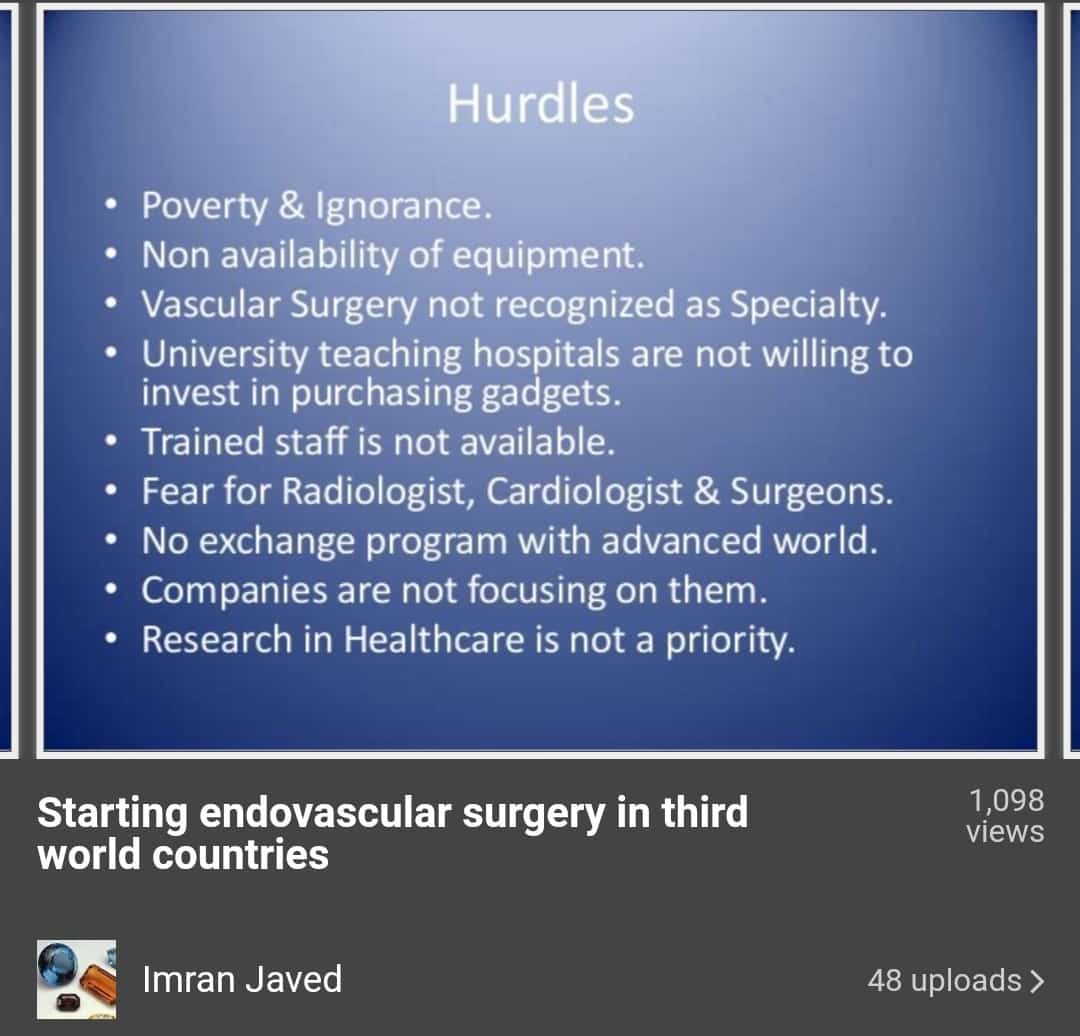
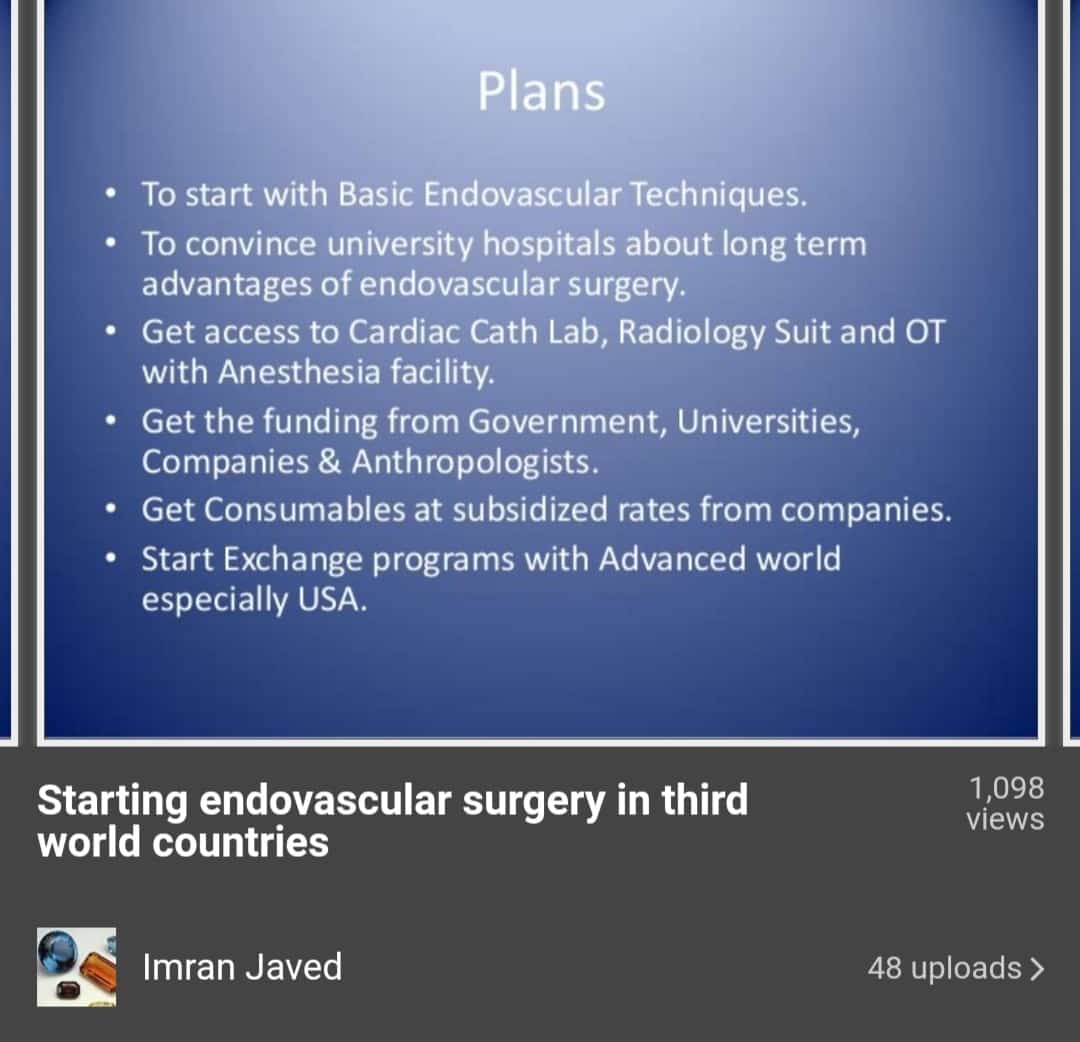
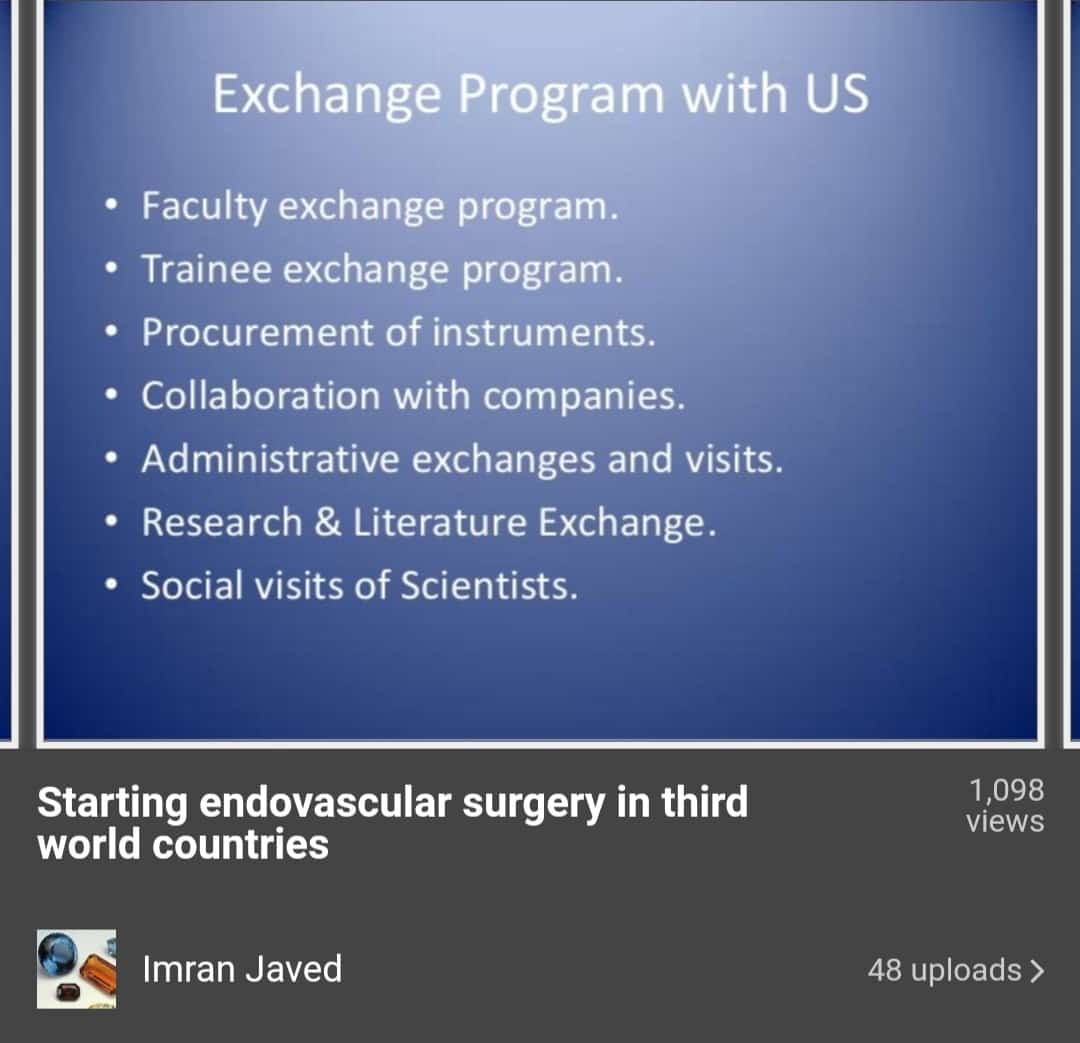
Dr. Imran Javed is the first physician who acquired this level of international training and start implementation in this part of world where medical facilities are not at an advanced level. Dr. Imran Javed is the first to Starting Endovascular Surgery in third World Countries Professor Dr. Imran Javed. MBBS, FCPS Surgery. Associate Professor of Surgery.
In 2006, when Dr. Imran Javed was working as Senior registrar Cardiac Surgery at Jinnah Hospital Lahore, came to know about the new specialization field, so he decided to opt for it as a future. Dr. Imran Javed contacted Arizona Heart Institue, Phonix, USA. In 2009, he got permission to enroll in the one-year advanced training program.
” Under the supervision of Dr. Edward and 6 members medical team of cardiac and vascular surgeon I started my pathway. During the first 3 months, I deeply understand the peripheral vascular interventions and later study about Abdominal and Thoracic Aorta interventions. last but not least portion consists of Carotid artery interventions and Mesenteric vessels” Dr. Imram Javed said:
Contact With Dr. Imran Javed
Following are the contact details for Dr. Imran Javed
Nawab Clinic Ali Pur Chatta “Nawab Street, Alipur Chatha, Gujranwala, Pakistan”
You can consult online with Dr. Imran Javed
Book Online Consultation here:
https://www.marham.pk/personal/6976
![]() nawabdin725@yahoo.com
nawabdin725@yahoo.com
![]() Whatsapp/SMS 0300-4897504
Whatsapp/SMS 0300-4897504

























Leave a Reply